
このページの監修医師

このページの監修医師
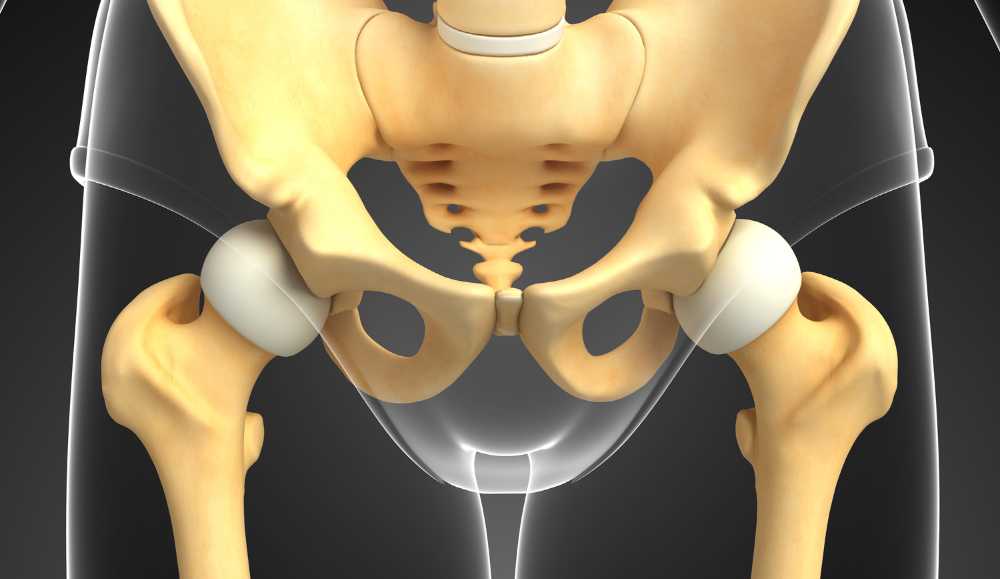
Treatment for uterine prolapse varies depending on the severity of the symptoms.
In mild cases, pelvic floor muscle training to strengthen weakened pelvic floor muscles, along with addressing issues like obesity and constipation, may improve the condition.
If the uterus is partially or completely prolapsed, the following treatments are performed:
* **Pessary Therapy:** A device called a pessary is inserted into the vagina to reposition the uterus within the pelvis and prevent prolapse. Since this involves inserting a foreign object into the vagina, symptoms such as vaginitis, increased vaginal discharge, and bleeding may occur. Therefore, regular check-ups with a healthcare professional are necessary for appropriate management. To prevent complications, pessaries need to be replaced periodically.
* **Surgical Treatment:** Surgical intervention is used for fundamental improvement. Several surgical options exist, including removing the prolapsed uterus through the vagina, suturing the loosened areas (bladder and rectal walls), reinforcing the vaginal wall with a mesh made of artificial material, and closing the vagina.
FemiCushion is a new medical device designed for the prevention and treatment of pelvic organ prolapse (including uterine prolapse, cystocele, rectocele, enterocele, etc.).
It is suitable for those who:
* Cannot use ring pessaries
* Cannot undergo surgery due to underlying health conditions
* Have difficulty visiting the hospital regularly
FemiCushion works by supporting the prolapsed organs. With the prolapsed organs returned to their normal position within the vagina, the cushion covers the vaginal opening, while the holder and supporter lift and hold the organs in place. It can be worn as needed by the user.
In addition to providing immediate relief from symptoms, FemiCushion prevents organ prolapse even under abdominal pressure, and it can be washed and reused. The design resembles underwear, making it discreet and unlikely to be recognized as a medical device by others.
A woman’s body goes through four main stages of aging: adolescence, sexual maturity, menopause, and old age. Although there are some individual differences, these are generally adolescence, sexual maturity, menopause, and old age. Menopause generally refers to the period around 45 to 55 years old, before and after menstruation stops. When women reach menopause, the secretion of female hormones (estrogen and ovarian hormones), which were abundant until then, decreases.
This disrupts hormonal balance, leading to various changes in the body. This is called “menopausal symptoms,” and if these symptoms hinder daily life, it is called “menopausal syndrome.” Many of you may have heard of menopausal syndrome. Genital pain is one of the typical symptoms of menopausal syndrome. It is said that about half of menopausal women experience genital pain. This indicates that many women suffer from genital pain and discomfort during menopause.
The main cause of this pain is vaginal dryness, which is highly likely to be a symptom of atrophic vaginitis.
As estrogen decreases with age, the vaginal walls and lining tend to become dry. Dryness thins the membrane, reduces vaginal secretions, and makes the vagina itchy and prone to inflammation.
Atrophic vaginitis is a condition in which the vaginal walls, which should normally be moist, become dry and irritated. The main symptoms include:
* Irregular bleeding
* Yellow or brown discharge
* Itching
* Pain
* Discomfort
* Pain during intercourse (dyspareunia)
* Cystitis
* Frequent urination
* Foul odor
* Pain during urination
The vagina contains about six types of resident bacteria that maintain a normal (acidic) vaginal environment and prevent the growth of pathogenic bacteria while menstruation occurs. This is called the self-cleaning function of the vagina.
However, after menopause, the number of these resident bacteria decreases. In addition to resident bacteria, female hormones (estrogen and ovarian hormones) also usually decrease. As a result, the cells that kept the vagina healthy also decrease and atrophy. At the same time, vaginal secretions also decrease, and with the decrease in collagen, the vagina loses moisture and becomes dry. Consequently, pathogenic bacteria can easily multiply, causing pain and bleeding even with slight stimulation.
Since menopause occurs naturally with age, atrophic vaginitis is also called senile vaginitis.
As mentioned above, the cause lies in the decline of female hormones (estrogen and follicular hormone) due to aging, which leads to dryness in the genital area. In other words, it’s a state of hormonal imbalance. A dry vagina becomes more susceptible to irritation, allowing bacteria to multiply and manifest various symptoms and discomfort. Common causes of hormonal imbalance include:
* Aging
* Smoking
* Post-cancer treatment
* Childbirth
* Breastfeeding
* Stress
* Unhealthy lifestyle
While our bodies produce plenty of hormones when we are young and healthy, production gradually decreases with age. Maintaining a youthful internal age through proper exercise and diet can help suppress poor physical condition and hormonal imbalances. Pay special attention to your diet.
Hormonal imbalances due to childbirth and breastfeeding usually stabilize with medication or time, but it is crucial to be mindful of smoking, stress, and unhealthy lifestyles. Smoking not only disrupts hormonal balance but also induces lung diseases and physical decline. It has been linked to cardiovascular diseases such as stroke and ischemic heart disease and contributes to diabetes and periodontal disease. Smoking also negatively affects those around you, so ideally, you should gradually reduce the number of cigarettes you smoke and eventually quit.
Stress, whether from a busy lifestyle, prolonged tension, or extreme temperature changes, can take many forms. Hormones are primarily produced under the brain’s command, and the human brain is highly sensitive and delicate when it comes to stress. Excessive stress can impair brain function, leading to hormonal imbalances. It’s beneficial to have a place where you can truly relax.
Furthermore, an unhealthy lifestyle, such as lack of sleep and overeating, also disrupts hormonal balance. Strive to maintain a regular lifestyle as much as possible. Sleep deprivation and overeating often stem from stress, so stress management is crucial.
Hormonal imbalances can cause various physical symptoms, such as dizziness, palpitations, headaches, and insomnia, similar to autonomic nervous system dysfunction. Many individuals also experience anxiety. Sometimes, it can even lead to other serious illnesses. Before your mind and body suffer significant damage, it’s crucial to maintain balance through diet, exercise, and relaxation.
Atrophic vaginitis is examined through an internal pelvic examination. The first step is to rule out serious conditions such as uterine or breast cancer. Eliminating the possibility of severe diseases can provide some relief to patients. Moreover, the risk of various cancers increases after the age of 40. Early detection allows for early treatment and can lead to a complete cure. Therefore, it is important to check for cancer first.
The internal examination doesn’t take long. Although you may feel nervous, try to relax and take deep breaths; it will be over quickly. The pain is not as severe as you might worry about, so please feel at ease during the examination.
The primary treatment is to supplement the deficient female hormones. Since the cause of the discomfort is the decrease in female hormones, replenishing them can improve the condition. Specifically, treatment involves estrogen preparations such as vaginal suppositories, patches, creams, and sometimes oral medications. While over-the-counter medications are available at drugstores, they have been reported to worsen symptoms in some cases, so it’s best to consult a medical professional.
The treatment period varies from person to person, but generally, improvement is observed within one to two weeks of starting the medication, and many cases improve within three weeks. However, due to the delicate nature of the area and the inevitable aging process, recurrence is possible, requiring further consultation.
FemiCushion is a product developed by Mitsui Medical Japan for the treatment of all types of pelvic organ prolapse, including uterine prolapse, cystocele, rectocele, and enterocele.

永尾 光一 先生
一般社団法人日本精索静脈瘤協会 理事長
医療法人社団マイクロ会 理事長
銀座リプロ外科 院長
昭和大学にて形成外科学を8年間専攻。その後、東邦大学で泌尿器科学を専攻し、形成外科・泌尿器科両方の診療科部長を経験する(2つの基本領域専門医を取得)。得意分野はマイクロサージャリーをはじめとする生殖医学領域の形成外科的手術。泌尿器科医の枠を超えた細やかな手術手技と丁寧な診察で、様々な悩みを抱える患者さんから高い信頼と評価を得ている。

株式会社三井メディカルジャパン 代表取締役
三井 桂子
株式会社三井メディカルジャパン 代表取締役。日本における女性疾患についての認知や理解度の低さに危機感をおぼえ、医療機器開発に着手。子宮脱をはじめとする骨盤臓器脱の治療に用いる「フェミクッション」を開発し、三井メディカルジャパンを通じて発売。
高齢者のむくみには弾性ストッキングが有効です。着用をおすすめするケースや弾性ストッキングの選び方を解説します。高齢者が着用を続けるためには、履きやすい商品を選ぶことが大切です。
続きを読む目次1 三井社長についての質問2 フェミクッション開発経緯3 三井社長の想い4 フェミクッションの効果・優位性4.1 当社の提携医療機関5 今後の展望6 患者さんへのメッセージ 三井社長についての質問 本日は、三井メ…
続きを読む50代を迎えて精神的な不調や腟の違和感が表れ始め、「更年期症状ではないか」と不安を感じていませんか。 エストロゲン(女性ホルモン)低下は加齢といった原因で起こり、多くの女性がさまざまな症状を経験します。…
続きを読む「子宮脱のような症状があるけれど、何科を受診すれば良いかわからない」とお困りではありませんか。 近年、女性特有の悩みである子宮脱のような骨盤臓器脱を治療できる診療科が増えてきています。しかし、骨盤臓器…
続きを読むスターターキット ライトネット購入限定

まずは試してみたい
という⽅に!
セット内容
・サポーター1枚(ミディベージュサポーター)
・クッション 3個(S・M・L各サイズ1個)
・布製ホルダー(フリーサイズ3枚)
・洗浄栓
※スターターキット ライトをご選択の方はミディベージュサポーターのみとなります。
スターターキット

普段の⽣活でしっかり
使いたい⽅に!
セット内容
・サポーター1枚(次の項目で種類・サイズを選択ください)
・クッション 6個(S・M・L各サイズ2個)
・布製ホルダー(フリーサイズ3枚)
・洗浄栓
※コットンの特注サイズは現在在庫切れです。