
このページの監修医師

このページの監修医師

Uterine prolapse is a condition that occurs when the uterus descends from its normal position into the vagina. In severe cases, the uterus may even protrude outside the vagina. This condition is often referred to as pelvic organ prolapse, as it involves the descent of pelvic organs.
Uterine prolapse is defined as the descent of the uterus into the vagina, but not outside of it. Specifically, it is diagnosed when the cervix descends below the line connecting the ischial spines, which are bony prominences on either side of the pelvis.
Studies have shown that the prevalence of uterine prolapse, including cases that have progressed to uterine prolapse, is 14% among women in general. However, many women with uterine prolapse do not experience any symptoms and therefore do not seek medical attention. This makes it difficult to accurately estimate the true prevalence of the condition. It is believed that the actual number of women with uterine prolapse is likely higher than the reported 14%.
The pelvic organs are supported by a group of muscles and ligaments called the pelvic floor. Uterine prolapse occurs when these muscles and ligaments become weakened or damaged, leading to the loss of support for the uterus. Several factors can contribute to the weakening of the pelvic floor, including:
* Pregnancy and childbirth: Vaginal delivery, especially multiple deliveries or deliveries of large babies, can strain and weaken the pelvic floor muscles.
* Obesity: Excess weight puts extra pressure on the pelvic floor.
* Aging: As women age, the pelvic floor muscles naturally weaken.
* Menopause: The decline in estrogen levels after menopause can contribute to the weakening of pelvic floor tissues.
* Chronic cough: Persistent coughing puts repeated strain on the pelvic floor.
* Chronic constipation: Straining during bowel movements can also weaken the pelvic floor.
* Heavy lifting: Repeatedly lifting heavy objects can put stress on the pelvic floor.
While various factors can contribute to uterine prolapse, the greatest risk factor is pregnancy and childbirth. The more vaginal deliveries a woman has, the higher her risk of developing uterine prolapse.
In its early stages, uterine prolapse often causes no noticeable symptoms. As the condition progresses, women may experience:
**Early symptoms:**
* A feeling of pressure or fullness in the pelvis
* A sensation of something “falling out” of the vagina
* Discomfort or pain during intercourse
* Low back pain
**Later symptoms:**
* Urinary incontinence or difficulty urinating
* Constipation or difficulty defecating
* Vaginal bleeding or discharge
* Protrusion of the uterus from the vagina
A pelvic exam is usually sufficient to diagnose uterine prolapse. During the exam, the doctor will visually inspect the vagina and cervix and may ask the patient to bear down to assess the degree of prolapse.
The treatment for uterine prolapse depends on the severity of the condition and the individual’s symptoms.
**Conservative treatment:**
* Lifestyle changes: Losing weight, avoiding heavy lifting, and treating chronic constipation can help prevent further prolapse.
* Pelvic floor exercises: Kegel exercises can strengthen the pelvic floor muscles.
* Pessary: A pessary is a device that is inserted into the vagina to support the uterus.
**Surgical treatment:**
* Vaginal hysterectomy: This procedure involves removing the uterus through the vagina.
* Vaginal repair: This procedure involves tightening the muscles and tissues of the vagina to support the uterus.
* Sacrocolpopexy: This procedure involves attaching the top of the vagina to the sacrum (the bone at the base of the spine) using surgical mesh.
With proper treatment, most women with uterine prolapse can experience significant improvement in their symptoms and quality of life. However, it is important to be aware that uterine prolapse can recur, especially if the underlying causes are not addressed.
Uterine prolapse is a common condition that can affect women of all ages. While it can be uncomfortable and even debilitating, there are effective treatments available. If you are experiencing symptoms of uterine prolapse, it is important to see your doctor for diagnosis and treatment.
The terms “uterine prolapse” and “uterine descent” are often used to describe the same set of symptoms, such as discomfort or a feeling of heaviness in the lower abdomen. However, the two terms are often used to distinguish between different degrees of the condition.
“Uterine prolapse” typically refers to cases where the uterus has descended into the vagina, while “uterine descent” generally describes a state where the uterus has descended but has not yet protruded from the vagina. In cases of uterine descent, lifestyle changes and pelvic floor exercises may be enough to improve symptoms without the need for surgery or devices. However, if the condition has progressed to uterine prolapse, treatment with a pessary or surgery may be necessary for prevention and treatment.
Pelvic organ prolapse (POP) is a condition in which organs normally supported by the pelvic floor muscles and ligaments (such as the uterus, bladder, urethra, small intestine, and rectum) descend and protrude from the vagina. This condition is also sometimes referred to as “genital prolapse” or “vaginal prolapse.”
POP can be further categorized based on the specific organ that has prolapsed, such as uterine prolapse, cystocele (bladder prolapse), and rectocele (rectal prolapse). However, it is common for multiple organs to prolapse simultaneously, which is why the term “pelvic organ prolapse” is increasingly used as a general term.
POP is not a rare condition and has been affecting women for centuries. It is more common in middle-aged and older women. Unfortunately, awareness of POP remains low, and many women suffer in silence due to embarrassment or uncertainty about which medical specialist to consult. However, it is important to seek medical attention from a gynecologist or urologist if you experience any symptoms, as POP does not resolve on its own.
Common symptoms of POP include:
* A feeling of a round object, like a ping pong ball, in the genital area (especially noticeable during bathing)
* A sensation of something descending or being pulled down in the lower abdomen or vagina
* A feeling of something being stuck between the legs
* Frequent urination
* Difficulty urinating or defecating
Symptoms often worsen throughout the day and are more pronounced in the afternoon after activity compared to the morning. In the early stages, the prolapse may only occur when straining, such as during a bowel movement. As the condition progresses, the prolapse may become more persistent and even protrude constantly, potentially causing friction against underwear and leading to bleeding. In severe cases, walking can become difficult, significantly impacting daily life.
The primary cause of POP is the weakening of the pelvic floor muscles and ligaments that support the pelvic organs. Chronic strain on the vagina can increase the risk of developing POP.
Factors that contribute to POP include:
* Multiple childbirths
* Aging
* Obesity
* Chronic constipation or coughing
* Occupations that involve prolonged standing or heavy lifting
Treatment for POP can be broadly divided into two categories: surgical and conservative. Medications are generally ineffective in treating POP.
Various surgical procedures are available to treat POP, and the specific approach will depend on the individual’s symptoms and the extent of the prolapse. Some common surgical procedures include:
* **Vaginal hysterectomy with anterior and posterior colporrhaphy:** This involves removing the prolapsed uterus through the vagina and reinforcing the fascia between the bladder and vagina with sutures. This traditional approach has a 30-40% chance of recurrence because it involves suturing already weakened tissues.
* **Transvaginal mesh surgery:** This involves using a mesh to reinforce the weakened fascia and ligaments. The mesh is typically made of a synthetic material like polypropylene and is also used in hernia surgeries.
A common conservative treatment for POP is pessary therapy. This is suitable for individuals with mild symptoms or those who cannot or do not wish to undergo surgery. A pessary is a device inserted into the vagina to support the uterus and/or bladder. It can be easily inserted and removed by the individual and is less invasive than surgery. Pessaries can help prevent complications like vaginitis and bleeding. However, they require regular replacement and do not address the underlying cause of the prolapse.
FemiCushion is a product developed by Mitsui Medical Japan for the treatment of all types of pelvic organ prolapse, including uterine prolapse, cystocele, rectocele, and enterocele.
It works by supporting the pelvic organs with a cushion at the vaginal opening and a holder and supporter that lift and hold the organs in place, preventing them from protruding when abdominal pressure increases. FemiCushion provides immediate symptom relief and allows individuals to live their daily lives with confidence.
The cushion is made of a special material that is comfortable against the vaginal opening. It is not inserted into the body or left in place, minimizing the burden on the organs and vaginal mucosa while preventing the progression of the prolapse.
FemiCushion offers several advantages:
* Easy to apply and remove by the individual when needed
* Discreet design that resembles underwear
* Reusable and easy to clean
FemiCushion was developed to help women who experience discomfort and difficulties due to pelvic organ prolapse (POP) and is ideal for the following individuals:
* Those who have difficulty using or do not wish to use ring pessaries
* Those considering surgery (for pre- and post-operative management and recurrence prevention)
* Those who have concerns about sexual activity (such as those who wish to have children or do not want their partner to know about their condition)
For more details about FemiCushion
FemiCushion is a Class I medical device approved in Japan for its effectiveness in treating pelvic organ prolapse.
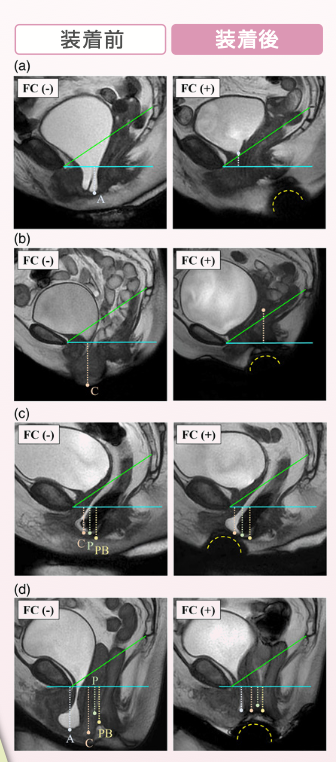
The MRI images below show (a) cystocele, (b) uterine prolapse, (c) enterocele and rectocele, and (d) complete eversion. In all cases, FemiCushion is identified as a hemisphere below the perineum (dotted line), and all prolapsed organs are supported at a significantly higher position when wearing FemiCushion, demonstrating its effectiveness in improving pelvic organ prolapse.
Source: Nomura Y, Yoshimura Y, et al: Magnetic resonance imaging evaluation of the effectiveness of FemiCushion in pelvic organ prolapse. J. Obstet. Gynaecol. Res., 48(5): 1255-1264, 2022.

永尾 光一 先生
一般社団法人日本精索静脈瘤協会 理事長
医療法人社団マイクロ会 理事長
銀座リプロ外科 院長
昭和大学にて形成外科学を8年間専攻。その後、東邦大学で泌尿器科学を専攻し、形成外科・泌尿器科両方の診療科部長を経験する(2つの基本領域専門医を取得)。得意分野はマイクロサージャリーをはじめとする生殖医学領域の形成外科的手術。泌尿器科医の枠を超えた細やかな手術手技と丁寧な診察で、様々な悩みを抱える患者さんから高い信頼と評価を得ている。

株式会社三井メディカルジャパン 代表取締役
三井 桂子
株式会社三井メディカルジャパン 代表取締役。日本における女性疾患についての認知や理解度の低さに危機感をおぼえ、医療機器開発に着手。子宮脱をはじめとする骨盤臓器脱の治療に用いる「フェミクッション」を開発し、三井メディカルジャパンを通じて発売。
目次1 三井社長についての質問2 フェミクッション開発経緯3 三井社長の想い4 フェミクッションの効果・優位性4.1 当社の提携医療機関5 今後の展望6 患者さんへのメッセージ 三井社長についての質問 本日は、三井メ…
続きを読む50代を迎えて精神的な不調や腟の違和感が表れ始め、「更年期症状ではないか」と不安を感じていませんか。 エストロゲン(女性ホルモン)低下は加齢といった原因で起こり、多くの女性がさまざまな症状を経験します。…
続きを読む「子宮脱のような症状があるけれど、何科を受診すれば良いかわからない」とお困りではありませんか。 近年、女性特有の悩みである子宮脱のような骨盤臓器脱を治療できる診療科が増えてきています。しかし、骨盤臓器…
続きを読むFemicushion™: UNICAMP – Urology Department – Campinas – Brazil 目次1 要旨1.1 導入と目的1.2 患者 […]
続きを読むスターターキット ライトネット購入限定

まずは試してみたい
という⽅に!
セット内容
・サポーター1枚(ミディベージュサポーター)
・クッション 3個(S・M・L各サイズ1個)
・布製ホルダー(フリーサイズ3枚)
・洗浄栓
※スターターキット ライトをご選択の方はミディベージュサポーターのみとなります。
スターターキット

普段の⽣活でしっかり
使いたい⽅に!
セット内容
・サポーター1枚(次の項目で種類・サイズを選択ください)
・クッション 6個(S・M・L各サイズ2個)
・布製ホルダー(フリーサイズ3枚)
・洗浄栓
※コットンの特注サイズは現在在庫切れです。